Welcome back, DERM Community!
Brrr... it’s getting chilly out there! As the weather shifts, so do our skin’s needs, and we’re here to help you stay ahead of the game. Whether you’re gearing up to guide your patients or just looking for ways to protect your own skin, this season calls for some serious TLC.
With the cold comes a familiar foe for many—eczema. Maybe you’ve seen a patient battling stubborn flare-ups or have a loved one desperate for relief from dry, irritated skin. Eczema isn’t just a skin condition; it’s a constant challenge that can impact comfort, confidence, and quality of life.
This week, in Beneath the Surface, we’re diving into the world of eczema. We’ll break down the basics, explore ways to fine-tune your diagnostic skills, and share management tips that really work. Our goal? To arm you with insights that make a difference in your clinical practice.
So, grab your coffee, cozy up, and let’s tackle eczema together. Get ready to turn challenges into opportunities for care and healing!
Featured on This Week’s Chapter:
🚀 Learning Opportunities: Eczema 101

Quick Overview: Why Eczema Matters
Eczema isn’t just about dry skin or an annoying itch. It’s a condition that goes skin-deep, affecting physical health, emotional well-being, and even daily routines. Those flare-ups? They’re more than an inconvenience—they’re a sign of a disrupted skin barrier and an overactive immune response. Understanding eczema means equipping yourself with the knowledge to bring relief and restore confidence to those affected.
Here’s what we’ll cover:
What is Eczema?
The Basics: Understanding eczema’s key features and classifications
Skin Timelines: How presentation evolves with time
Breaking Down the Stages + Treatment
Triggers and Treatments: Personalized Approaches
Id Reactions: Secondary Rashes from Primary Issues
10 Simple Treatment and Prevention Tips for Eczema
What is Eczema?

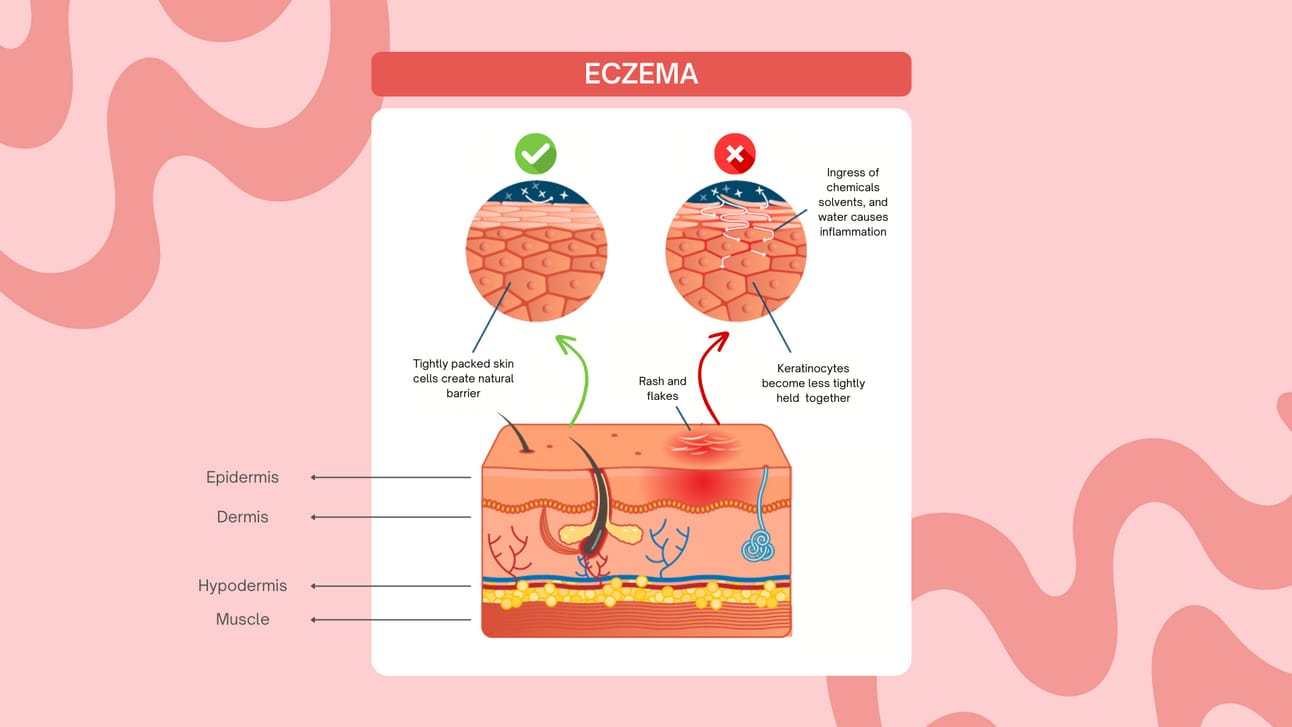
Eczema is a term used to describe a variety of skin conditions that cause redness, itching, and inflammation. You might have heard it called "atopic dermatitis," which is the most common form. It's more than just dry skin; eczema can make your skin feel itchy, scaly, and even cracked. The good news is, while it can be a persistent condition, there are plenty of treatments available to help manage flare-ups.
Eczema tends to happen when your skin's natural barrier is weakened, allowing irritants and allergens to enter more easily. This can be triggered by things like stress, allergens (like dust or pet dander), or even certain soaps or fabrics. So, if you’ve been dealing with irritated, itchy skin, you're not alone! It's important to know that eczema isn't contagious—meaning, you can’t catch it from someone else, and people around you can't "get" it from you.
Managing eczema often involves a mix of good skincare routines, like moisturizing regularly, and avoiding triggers that can make symptoms worse. So, if eczema is something you're living with, don’t worry—there’s hope in getting your skin feeling better again!
The Basics: Understanding the Different Types of Eczema
Eczema isn’t one-size-fits-all—it can show up in several different ways, and each type has its own unique features and triggers. Here’s a quick rundown of the seven main types:
Atopic Dermatitis: This is the most common type, causing inflammation, dryness, and itchy skin. While it’s often seen in children, it can show up at any age.
Contact Dermatitis: Also known as allergic contact dermatitis, this type is triggered by environmental factors like certain chemicals or plants that come into contact with your skin.
Dyshidrotic Eczema: This one causes dry skin, along with a burning sensation, rashes, and itchy blisters, usually on the hands and feet.
Neurodermatitis: Also called discoid eczema, this form affects small patches of skin, making them itchy and scaly. It can be triggered by repeated scratching.
Nummular Eczema: This type creates round, coin-shaped lesions, often on the arms and legs. It can be especially frustrating because it looks different from other forms of eczema.
Seborrheic Dermatitis: Often affecting your scalp, seborrheic dermatitis causes inflammation and flakes, leading to a scaly, red rash. It’s more than just dandruff!
Stasis Dermatitis: This one appears on the legs, often looking like skin discoloration or varicose veins, and is related to poor blood flow.
It’s important to note that you can have more than one type of eczema at the same time! Each form has its own set of triggers and treatment needs, which is why it’s crucial to talk to a healthcare professional. Dermatologists can help pinpoint which type or types of eczema you may be dealing with and guide you on how to manage it effectively.
Skin Timelines: How Presentation Evolves Over Time
Eczema symptoms and appearances change as a person ages:
Infancy: Red, weepy patches often found on the cheeks and scalp.
Childhood: Thickened skin with pronounced lines, commonly in flexural areas.
Adulthood: Persistent dryness, lichenification, and more widespread involvement.
Tracking these changes helps tailor treatment at every stage of life.
Breaking Down the Stages + Treatment

When treating eczema, it's important to focus on restoring the skin's natural barrier, educating both the patient and their family, and identifying the root cause of any flare-ups or chronic exacerbations.
*Itching (pruritus) is a common symptom throughout, so relief from this discomfort is key.
Topical Steroid (TS) Considerations
For the face, groin, and axillae, avoid using fluorinated TS.
You can use fluorinated TS on other areas of the body where needed.
Be cautious with TS on areas showing signs of thinning or steroid atrophy.
Avoid using super-potent TS in infants and young children.
—————
Acute Dermatitis
Diagnosis (DX):
Look for vesicles, oozing, swelling, crusting, and redness.
Treatment (TX):
Wet-dry compresses (like Domeboro or vinegar/water solutions) can help remove exudative crusts.
Apply topical TS in the form of sprays, creams, or foams, and use stronger classes when possible.
For more severe cases, a short course of oral corticosteroids alongside TS might be helpful.
—————
Subacute Dermatitis
Diagnosis (DX):
You'll notice juicy papules and redness.
Treatment (TX):
Topical TS will help control inflammation.
Calcineurin inhibitors can also be effective in reducing flare-ups.
—————
Chronic Dermatitis
Diagnosis (DX):
Look for plaques, scales, thickening of the skin (lichenification), pigmentation changes, lichen simplex chronicus (LSC), excoriation, crusting, and fissures.
Treatment (TX):
Topical TS ointments are great for drier, thicker plaques.
For best results, try occluding with kitchen wrap at bedtime to enhance absorption.
Calcineurin inhibitors may still be effective.
A short course of oral corticosteroids can be considered for persistent cases.
If there's a secondary infection, antibiotics will be necessary.
For stubborn plaques, intralesional injections of Kenalog (Triamcinolone) at 2.5-3 mg/cc, spaced 1 cm apart, can help clear the affected areas.
Triggers and Treatments: Personalized Approaches
Identifying triggers is crucial for managing eczema. Common culprits include:
Environmental Factors: Dry air, harsh soaps, allergens.
Dietary Elements: Certain foods may exacerbate symptoms in some patients.
Treatment strategies focus on:
Restoring the skin barrier with emollients and moisturizers.
Reducing inflammation with appropriately chosen topical steroids.
Managing itching and preventing infections.
Id Reactions: Secondary Rashes from Primary Issues
An id reaction is a type of secondary skin reaction that occurs when the body develops a rash in response to an existing primary skin condition or infection. Essentially, the primary issue causes a widespread, often more generalized, rash in areas of the body that were not initially affected.
For example:
A fungal infection might trigger eczema-like lesions on distant parts of the body.
Severe contact dermatitis can provoke a systemic skin response, causing rashes on other areas of the skin.
In short, an id reaction happens when the body’s immune system responds to the original skin problem, and addressing the underlying cause of the primary condition is key to resolving the secondary rashes.
10 Simple Treatment and Prevention Tips for Eczema
Moisturize Regularly: Use fragrance-free, thick creams or ointments to lock in moisture, especially after bathing.
Avoid Scratching: Scratching can worsen eczema and lead to infection. Use cool compresses or anti-itch creams instead.
Use Mild, Fragrance-Free Soaps: Harsh soaps can irritate the skin. Choose gentle, fragrance-free options for bathing.
Apply Topical Steroids: Use prescribed steroids to reduce inflammation during flare-ups. Be cautious with strong steroids on sensitive areas like the face.
Wear Soft, Breathable Fabrics: Cotton is best. Avoid wool or synthetic fabrics that can irritate the skin.
Avoid Hot Showers: Hot water can dry out the skin. Opt for lukewarm showers and limit time spent in water.
Maintain Cool Temperatures: Hot weather or extreme cold can trigger eczema flare-ups. Keep your environment cool and moisturized.
Identify and Avoid Triggers: Common triggers include allergens like dust, pet dander, or certain foods (see below for foods to avoid).
Use Wet Wraps for Severe Flare-Ups: For more severe eczema, wrapping moisturizers or prescribed creams with a damp cloth can help soothe and hydrate the skin.
Consult a Dermatologist for Persistent Cases: If eczema doesn’t improve with home care, seek professional advice for more advanced treatments like calcineurin inhibitors or oral medications.
—————
Foods to potentially avoid, if a food allergy is suspected:
Dairy (milk, cheese, yogurt)
Eggs
Nuts (peanuts, tree nuts)
Soy
Gluten (wheat, barley, rye)
Citrus fruits (lemons, oranges)
Spicy foods
Artificial additives and preservatives
—————
Creams to Apply:
Hydrocortisone (mild steroid) for flare-ups.
Calcineurin inhibitors (e.g., tacrolimus, pimecrolimus) to reduce inflammation without steroids.
Emollients (e.g., Aquaphor, Eucerin) to lock in moisture.
Anti-itch creams containing menthol or pramoxine to soothe itching.
—————
What to Do in Certain Cases:
Infection: If eczema becomes infected, consult a doctor for antibiotic creams or oral antibiotics.
Severe Flare-Ups: Consider using stronger topical steroids or oral corticosteroids as prescribed by a healthcare provider.
Chronic Eczema: Follow a consistent skincare routine and keep stress levels in check, as stress can worsen flare-ups.
Every patient interaction is an opportunity to manage eczema effectively. By understanding triggers, treatment options, and skincare routines, you can empower patients to take control of their condition and improve their quality of life.
Looking to expand your knowledge? Explore our advanced CE module, ‘Eczema,’ for expert strategies designed for dermatology professionals.
📚 Why Choose Us for Your Continuing Education?
For all healthcare practitioners:
↳ Flexible learning: Fit your studies around your schedule.
↳ Real-world impact: Elevate your care with the latest in dermatology.
Earn your CE credits with one of the greatest educational platforms across the U.S.
🔎 Research Highlight
The impact of temperature on the skin barrier and atopic dermatitis
Hui-Beckman, J. W., Goleva, E., Leung, D. Y. M., & Kim, B. E.
Climate change is affecting public health worldwide and worsening many diseases, including atopic dermatitis (AD), allergies, infections, heart conditions, injuries, and mental health issues. Over the years, cases of AD have increased, with changes in the environment, like shifting temperatures, playing a role.
Research shows that extreme temperatures—both very cold and very hot—can harm the skin barrier and trigger or worsen AD. For example, studies from different countries found that children born during colder seasons, such as fall and winter, are more likely to develop AD. Changes in temperature have also been linked to itching, skin flare-ups, more frequent doctor visits, and even asthma attacks.
Cold and hot weather cause the body to release certain chemicals, like interleukin-1β and prostaglandin E2, which lead to inflammation, itching, and skin problems. These processes also activate specific proteins in the skin, called TRP (Transient Receptor Potential) channels, which make symptoms like itching and flare-ups worse. Scientists are exploring treatments, such as TRPV (Transient Receptor Potential Vanilloid) blockers, that may help reduce these temperature-related effects on the skin.
Understanding how temperature affects AD is key to finding better ways to prevent and treat this condition, especially as climate change continues to influence our environment.
👋🏻 Until next time!
Thanks for tuning in to Beneath the Surface.
We’re grateful to have you on this journey with us, where expert insights meet real-world application in dermatology.
Let’s continue to learn, grow, and innovate together to advance the field and provide the best care for our patients.
Stay curious, stay connected, stay DERM!
— The Derm for Primary Care Team
