Welcome back, DERM Community!
Last week, we explored five unexpected situations dermatologists face in the clinic. Want to know how to respond with smart, ethical, and evidence-based decisions? Then check it out.
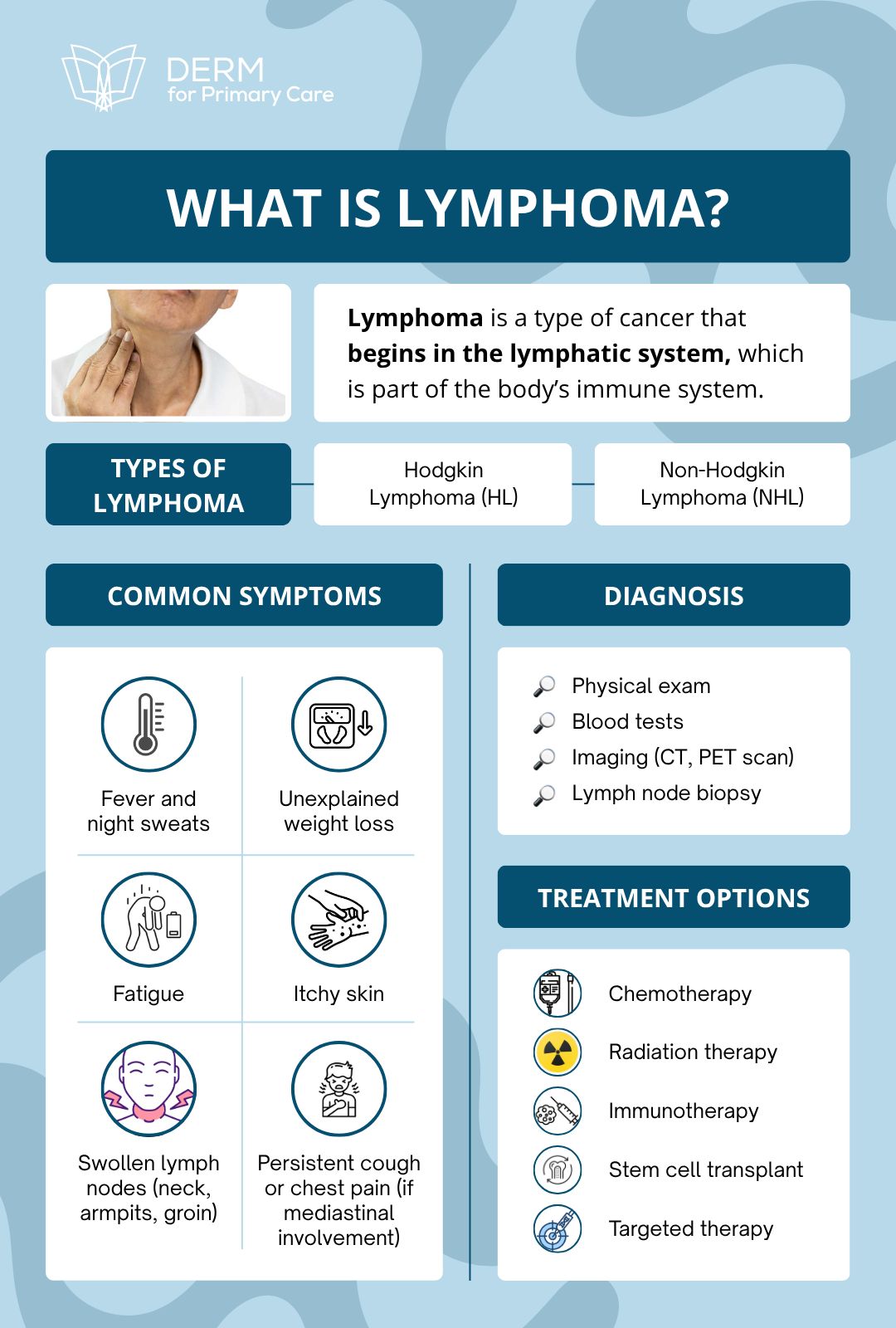
This week in Beneath the Surface, we’re diving into a diagnosis that often starts in your exam room: Lymphoma, as seen in one of our courses.
Let’s unpack five key ways lymphoma can show up in dermatology and how to think and act when it does.
Featured on This Week’s Chapter:
Learning Opportunities:
Cutaneous Lymphoma 101: What Every Derm Should Know
Cutaneous lymphoma is a spectrum of malignancies that primarily affect the skin. While the name might sound ominous, many cases follow an indolent course, making early diagnosis and monitoring critical.
🔬 Common Clues That Should Raise Your Suspicion
Treatment-Resistant Patches or Plaques
A red flag: lesions that look like eczema or psoriasis but don’t respond to topical steroids, antifungals, or other standard therapies.
These patches may wax and wane over years before progressing.Lesion Evolution Over Time
A spot that starts flat and scaly, then slowly thickens or forms nodules? That's a biopsy waiting to happen.
Unusual Distribution or Color
Hypopigmented patches, especially in younger patients or people with skin of color, can be early-stage CTCL. Poikiloderma (areas with mixed pigmentation, atrophy, and telangiectasias) is another red flag.
Disproportionate Itching
When the itch is severe but the inflammation seems mild, consider that you may be looking at more than dermatitis.Localized Nodules or Tumors on Normal Skin
This is more suggestive of CBCL. These lesions may appear on the face, scalp, or trunk, and grow slowly but persistently.
Opportunities for Dermatologists: Grow Your Career
👋🏻 See you next Thursday, DERM community!
Cutaneous lymphoma might not be on your radar every day, but keeping it in mind could save a patient months or even years of misdiagnosis.
The key is curiosity, consistency, and a commitment to digging deeper when the skin tells a story you’ve heard before, but something feels off.
Was this issue helpful? Forward it to a colleague, or share your feedback: we love hearing from you.
Have a topic you’d like us to cover next? Drop a comment below or reply to this email. Your input helps us shape a better learning experience for everyone.
Smart skin care starts with science. Feel good, look great, and keep glowing with evidence-based choices
— The Derm for Primary Care Team


