Welcome back, DERM Community!
Last week, we pulled back the curtain on herpes, one of the most stigmatized yet misunderstood conditions in dermatology. Missed it? Don’t worry: you can still catch up on the red flags and myths that matter.
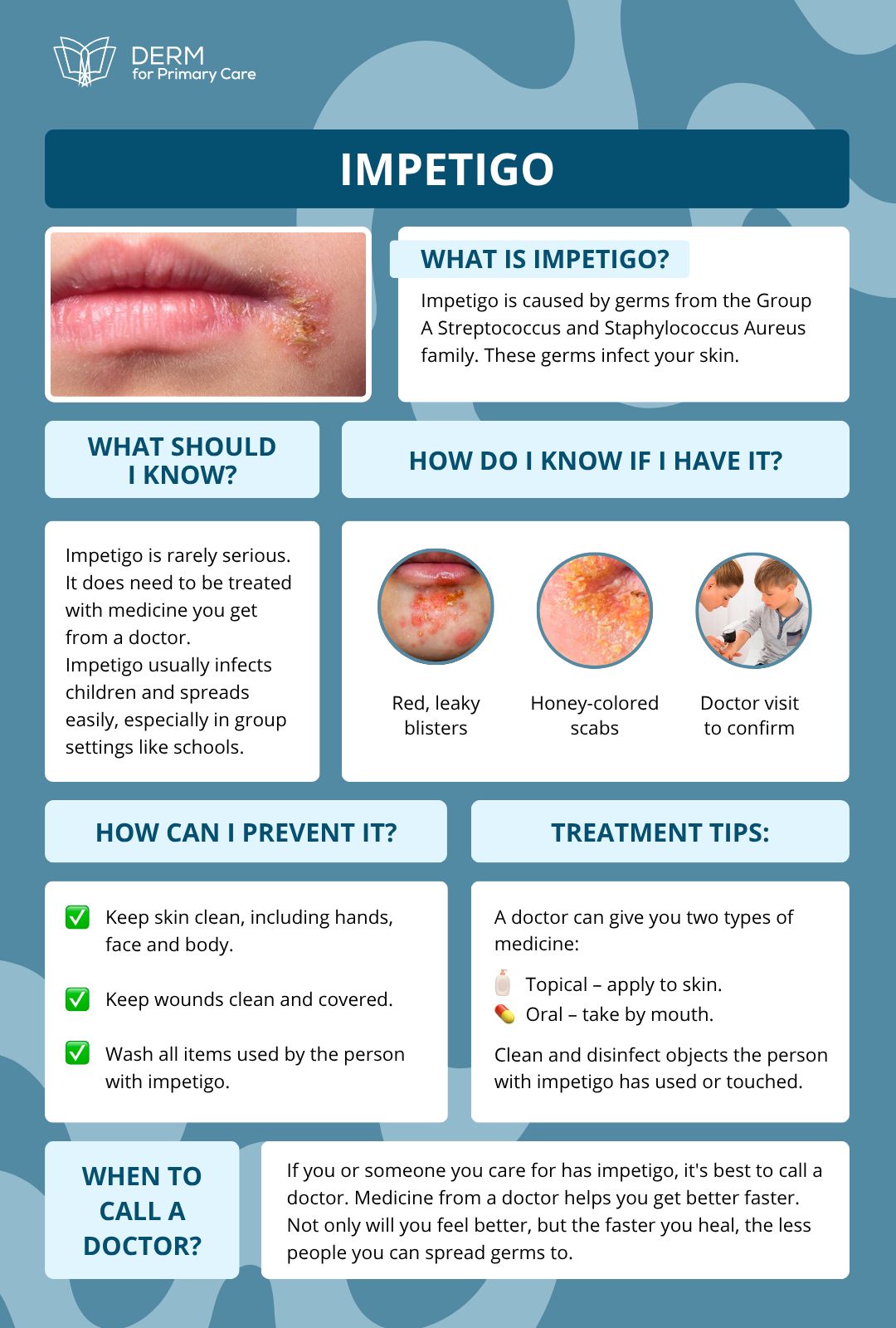
This week in Beneath the Surface, we’re focusing on Impetigo, a disease that can be overwhelming and scary. In our course we dive deep into real clinical cases, but today, let’s start with the essentials.
Featured on This Week’s Chapter:
What is Impetigo?
It is a deceptively simple infection that continues to challenge clinicians, especially when it mimics other dermatologic conditions or goes unrecognized in adults.
Whether it’s classic honey-colored crusts or subtle bullae, impetigo is more than “just a kid’s rash” and it deserves a closer look.
How It Spreads
Impetigo is highly contagious and spreads through:
Direct skin contact with infected lesions
Fomites like towels, bedding, or toys
Auto-inoculation from scratching
It thrives in settings like schools, daycares, and athletic teams, especially with poor hygiene or skin barrier disruptions (such as eczema, insect bites, minor trauma).
Why Recognizing It Matters
Impetigo isn’t just a nuisance, it can lead to complications such as:
Post-streptococcal glomerulonephritis
Cellulitis or deeper skin infections
MRSA transmission in community settings
And it’s often misdiagnosed as:
HSV (especially bullous impetigo)
Contact dermatitis
Tinea infections
Atopic eczema flare-ups
Early diagnosis is key to:
Starting topical or systemic antibiotics promptly
Preventing outbreaks in household or school settings
Avoiding unnecessary treatments or workups
Keep an eye out for rapidly spreading lesions, crusting, and mild pruritus or discomfort, especially when they appear in clusters or after minor trauma. Swabbing for culture may help when lesions are atypical or treatment fails.
Too much information?
Here’s a FREE guide for you to check it out later or share with your patients:
👋🏻 See you next Thursday, DERM community!
Impetigo may seem straightforward, but its clinical mimics, public health implications, and potential complications make it a condition worth mastering.
By staying sharp in your recognition, treatment, and prevention strategies, you’re not just curing skin, you’re curbing spread and protecting communities.
Seen an impetigo case that threw you off? A resistant bug that challenged your go-to treatment plan?
Hit reply, we want to hear your stories and may feature them in an upcoming issue.
Stay sharp, stay curious, and help patients feel seen, not judged.
— The Derm for Primary Care Team



