Welcome back, DERM Community!
Often underestimated, the skin isn’t just a protective layer —it’s a complex, dynamic organ essential to overall well-being.
As the days grow shorter and the chill settles in, winter brings a unique set of challenges for our skin. From battling the dryness caused by indoor heating to safeguarding against the icy winds outside, this season demands extra care and attention for our largest organ, the skin.
In this fourth issue of Beneath the Surface, we’ll guide you through essential insights to help your patients maintain healthy, resilient skin all year long. Let’s explore the fundamentals of skin science and health.
Bundle up, grab your favorite hot beverage, and let’s dive in!
Featured on This Week’s Chapter:
🚀 Learning Opportunities: Skin Science 101

Quick Overview
Did you know that your skin’s barrier is like a superhero in disguise? 🦸🏻. It works tirelessly to protect you from all sorts of threats, like bacteria, pollutants, and dehydration. When it's working well, it’s a smooth operator, keeping things calm and collected. But when it's compromised? Well, things can get a little messy, from irritation to infections.
Here’s what we’ll cover:
Understanding the Basics of Healthy Skin
The Structure and Function of the Skin Barrier
Factors That Weaken the Skin Barrier
Common Conditions Associated with a Damaged Skin Barrier
Treatment and Prevention Strategies (Even During Winter! ☃️
Understanding the Basics of Healthy Skin
The skin is the largest organ in your body, covering an impressive 2 square meters (2m²) and performing a multitude of essential functions that are critical for overall health. Here’s why the skin plays such an important role:
First Line of Defense: Your skin is the body’s primary defense against external threats like toxins, infections, and harmful UV radiation.
Temperature Regulation: Blood vessels and sweat glands in the skin help regulate body temperature. When you're hot, cutaneous blood vessels dilate, allowing heat to escape. When you're cold, blood vessels constrict, and you produce less sweat to conserve heat.
Sensory Function: Skin’s nerve endings and receptors allow you to sense touch, pain, and pressure, and help differentiate between hot and cold.
Critical Barrier Function: The skin’s barrier function is crucial for survival, protecting you from extreme temperatures, toxins, and infections. A weakened barrier can lead to severe conditions, like widespread full-thickness burns, which result in high mortality rates.
Dermatologic Therapy: One of the key goals of dermatologic treatments is to maintain, and when necessary, restore the skin’s natural barrier function, ensuring its protection and proper functioning.
The Structure and Function of the Skin Barrier

Skin Layers: Epidermis, Dermis, and Subcutaneous Tissue
The skin has two main layers: the epidermis and the dermis, plus a layer of subcutaneous fat beneath them.
Thickness varies depending on the area:
Epidermis: Thinnest on the eyelids (0.05mm) and thickest on the palms and soles (1.5mm).
Dermis: Thin on the eyelids (0.3mm) but thicker on the back (4mm or more).

Surface Layers of the Epidermis
Stratum Corneum: The outermost layer, acting as the skin's primary physical barrier. It’s thicker in areas like the palms and soles (up to 100 layers) and thinner elsewhere (10-25 layers).
Granular Layer: Contains more differentiated keratinocytes with granules that help maintain skin integrity.
Spinous Layer: This is where keratinocytes produce keratin, a key protein for skin strength.
Basal Layer: The deepest layer, containing the "stem cells" that regenerate skin cells.
Pigmentation and Melanocytes
Melanocytes in the basal layer produce melanin, the pigment responsible for skin color.
While the number of melanocytes is roughly the same across all skin types, the size, number of melanosomes (pigment-containing granules), and their distribution vary. For instance, darker skin has larger and more melanosomes, which provide more pigmentation.
Sunlight triggers melanocytes to increase melanin production, leading to a tan.
The Dermis: Strength, Support, and Function
The dermis provides structure and contains:
Collagen and elastin: These proteins give skin its strength and flexibility.
Blood vessels and nerves: Crucial for nourishment and regulating temperature.
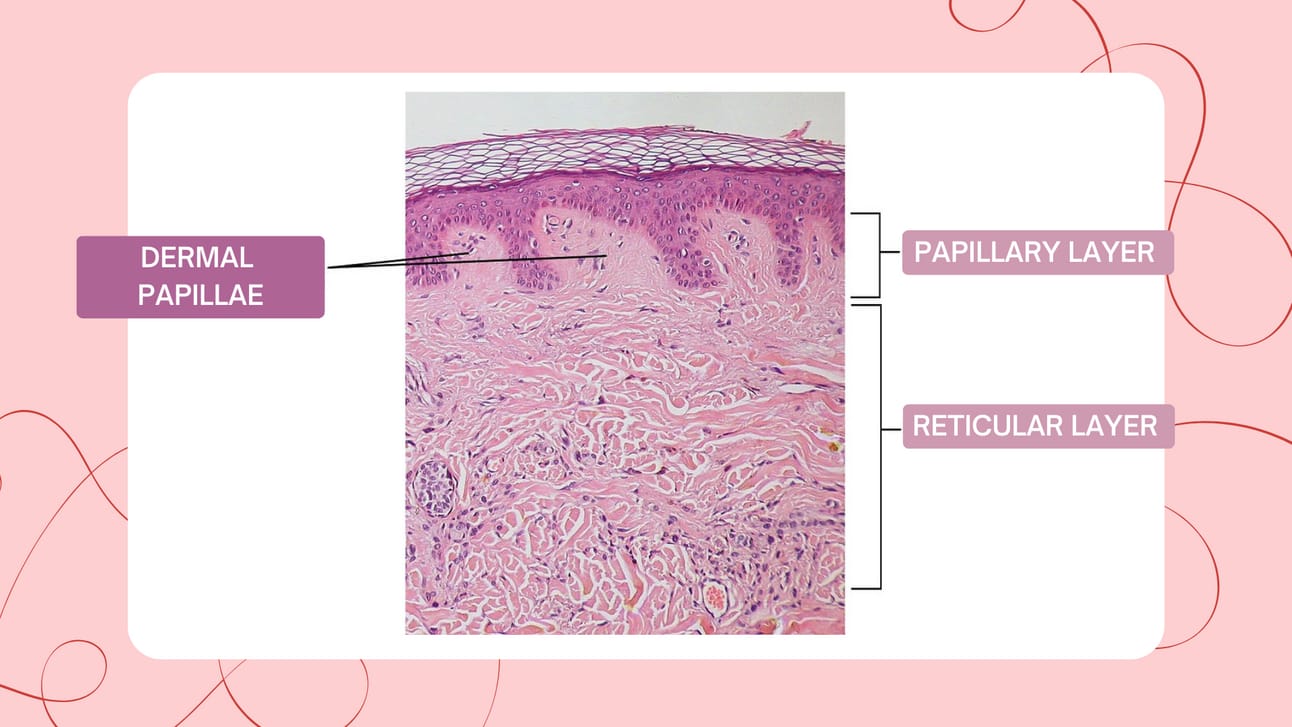
The dermis is made up of two layers:
Papillary Dermis: The upper part with loosely arranged collagen fibers.
Reticular Dermis: The lower part, thicker and with more densely packed collagen fibers.
Sebaceous Glands: Lubrication and Protection
Sebaceous glands secrete sebum, a lipid-rich substance that keeps your skin moisturized and protected.
These glands are most concentrated on the face, and their function is androgen-dependent, meaning they become more active during puberty.
Skin Appendages: Sweat, Hair, and Nails
Eccrine glands: These sweat glands are found almost everywhere on the body and play a key role in temperature regulation by releasing water and salt.
Apocrine glands: Located mainly in the armpits and groin, these sweat glands produce a substance that, when broken down by bacteria, causes body odor.
Hair and nails: Both are made of keratin, a protein that provides strength and protection to the skin.
The Skin's Immune System
The epidermis contains immune cells like keratinocytes, which release cytokines (immune system signals) and Langerhans cells, which present antigens.
The dermis houses the majority of the lymphocytes, which are responsible for fighting off infections and pathogens.
The interaction between epidermal and dermal immune cells ensures your skin can respond effectively to environmental threats like toxins, microbes, and other stressors.
Your skin is a dynamic, multi-functional organ that’s constantly working to protect you. Understanding its layers and functions can help you care for it better, especially during challenging weather conditions or when addressing skin concerns.
Factors That Weaken the Skin Barrier
The skin barrier doesn’t stay strong on its own —several external and internal factors can compromise its function. When the skin barrier is impaired, the skin becomes more vulnerable to dryness, irritation, infection, and even conditions like eczema, acne, and psoriasis.
Key Factors That Weaken the Skin Barrier:
Harsh Skincare Products: Overuse of products like exfoliants, toners with alcohol, and soaps with harsh ingredients can strip away essential lipids, leaving the skin vulnerable.
Environmental Stressors: Excessive sun exposure, pollution, and cold weather can damage the lipid barrier, making the skin more susceptible to irritation and infection.
Over-cleansing or Scrubbing: Frequent washing, especially with hot water, can dehydrate and irritate the skin, causing barrier damage.
Dietary Deficiencies: Poor nutrition, particularly a lack of omega-3 fatty acids and vitamins A and E, can lead to a compromised barrier.
Medical Conditions: Conditions like eczema, psoriasis, and rosacea are often linked to an impaired skin barrier.
Age: As we age, the skin naturally loses moisture and the production of lipids decreases, resulting in a thinner, more fragile skin barrier.
Common Conditions Associated with a Damaged Skin Barrier

When the skin barrier is weakened, the skin becomes more vulnerable to various conditions. A compromised barrier is often at the root of many common dermatological conditions.
Atopic Dermatitis (Eczema): A common condition where the skin becomes inflamed, itchy, and irritated, often due to a damaged skin barrier.
Acne Vulgaris: A weakened skin barrier allows bacteria like P. acnes to thrive, leading to inflammation and breakouts.
Psoriasis: This chronic autoimmune condition leads to thickened skin and scaly patches, often due to a damaged barrier.
Rosacea: A disorder where blood vessels under the skin enlarge, often exacerbated by a compromised barrier, leading to redness and inflammation.
Dry, Sensitive Skin: A compromised barrier leads to transepidermal water loss (TEWL), which results in dry, flaky, and sensitive skin.
Treatment and Prevention Strategies (Even During Winter! ☃️)
The Skin Barrier is the Foundation of Skin Health
A healthy skin barrier is vital for protection against environmental stressors and maintaining hydration.
The skin naturally regenerates to restore its barrier function.
The acid mantle, a slightly acidic film on the skin (pH 4.5–6.2), supports this barrier and promotes healthy microflora like S. epidermidis.
Key Strategies for Skin Health
Gentle Care and Hydration
Use hydrating products with ceramides, urea, lactic acid, and hyaluronic acid to restore the barrier.
Apply moisturizer 3–5 minutes after bathing, blotting the skin dry instead of rubbing. Start with blander products before those that might irritate (e.g., salicylic acid or ammonium lactate).
Avoid Harsh Practices
Over-cleansing and hot showers can strip the skin of essential oils and weaken the barrier. Opt for gentle, non-stripping cleansers.
Look out for common allergens in moisturizers, such as fragrances, parabens, and essential oils, as these can cause sensitivity or allergic contact dermatitis (ACD).
Hydration and Humectants
Humectants, like those in the skin’s natural moisturizing factor (NMF), attract and hold water. These substances include amino acids, urea, and lactic acid.
Reduced NMF (Natural Moisturizing Factor) is linked to dryness, cracking, and conditions like eczema or psoriasis. Using NMF-containing moisturizers helps restore hydration effectively.
Environmental and Nutritional Considerations
Cold, dry air in winter can exacerbate skin issues. Suggest humidifiers and adjustments to skincare routines for seasonal changes.
Encourage a balanced diet rich in omega-3 fatty acids and vitamins A, C, and E to boost skin health from within.
Customized and Consistent Care
Every patient’s skin is unique. Tailor treatments based on individual skin types, lifestyles, and concerns.
Reinforce the importance of a consistent skincare routine, focusing on gentle cleansing, hydration, and barrier repair for long-term success.
Long-Term Outlook
Healing the skin barrier requires patience —it can take weeks to see significant improvements.
Chronic symptoms like persistent redness or dryness may signal underlying conditions and should be explored further with an expert.
The skin barrier is your first defense against the world around you, and keeping it strong is essential for overall skin health. By recognizing the factors that compromise the barrier, adopting proper skincare habits, and incorporating the right products, you can help patients maintain their skin’s health and resilience.
↳ Ready to deepen your knowledge of skin science and elevate your expertise? Explore our CE course ‘Maintaining Healthy Skin’, for an in-depth dive into proper care for different skin types. Learn about the role of soaps, moisturizers, and shampoos, the basics of UV radiation, tanning, sunburn, and sun protection. Equip yourself with the insights you need to diagnose, treat, and support your patients on their journey to healthier, more resilient skin. 🧑🏻⚕️
📚 Why Choose Us for Your Continuing Education?
For all healthcare practitioners:
↳ Flexible learning: Fit your studies around your schedule.
↳ Real-world impact: Elevate your care with the latest in dermatology.
Earn your CE credits with one of the greatest educational platforms across the U.S.
🔎 Research Highlight
AI in Aesthetic/Cosmetic Dermatology: Current and Future
Thunga, S., Khan, M., Cho, S. I., Na, J. I., & Yoo, J.
Recent advancements in artificial intelligence (AI) have made significant strides in dermatology, especially in the diagnosis of skin diseases such as skin cancer. However, aesthetic dermatology presents unique challenges due to the subjectivity of traditional evaluation methods and the lack of standardized assessment tools.
This review examines the current state of AI in dermatology, highlights its potential in diagnosing skin conditions, and discusses the limitations of traditional aesthetic dermatology methods. Emerging AI technologies show promise but face challenges such as biased datasets and inconsistent evaluation standards.
To fully integrate AI into aesthetic dermatology, it is essential to develop standardized evaluation methods, collect diverse datasets, and educate practitioners on AI's capabilities and limitations. Overcoming these obstacles will improve diagnostic accuracy and patient outcomes, enabling more effective use of AI in clinical practice.
👋🏻 Until next time!
Thanks for tuning in to Beneath the Surface.
We’re grateful to have you on this journey with us, where expert insights meet real-world application in dermatology.
Let’s continue to learn, grow, and innovate together to advance the field and provide the best care for our patients.
Stay curious, stay connected, stay DERM!
— The Derm for Primary Care Team
