Welcome back, DERM Community!
We’re so excited to bring you another edition of Beneath the Surface.
Our goal? To keep you in the loop and inspired as you grow your dermatology expertise.
This is where you need to be: whether you’re just starting out as a Nurse Practitioner, leveling up as a Physician Assistant or Primary Care Physician, or taking your career as a Registered Nurse to new heights, we’ve got your back on this journey from learning to doing.
This is our second issue of practical tips, the latest trends, and tools to boost your clinical know-how —delivered straight to your inbox.
In case you missed our previous newsletter…
Here’s What to Expect in Our Issues:
🚀 Learning Opportunities: Snippets from our accessible online dermatology training courses. All healthcare practitioners are welcome to learn!
💭 Expert Q&A: Short interview with a top voice in the field. They share their career path and advice for newcomers and answer reader-submitted questions.
💼 Career Development: Networking. Job alerts. Connect with your peers —NPs, PAs, PCPs, or MDs. Actionable negotiation tips. Interview prep. Everything you need to take the plunge toward success.
🧑🏻⚕️ Resident Spotlight: Meet your peers making strides in dermatology.
🌎 Upcoming Dermatology Events: Discover seminars and conferences across the U.S.
Featured on This Week’s Chapter:
🚀 Learning Opportunities: Common Bacterial Skin Infections (Bacterial Folliculitis)
What You’ll Learn:
How to identify Bacterial Folliculitis, a common skin infection
Key signs, symptoms, and physical exam findings
Effective treatment strategies for mild and severe cases
Prevention tips to reduce recurrence
Quick Overview
Bacterial Folliculitis is an infection that involves hair follicles, often caused by Staphylococcus aureus. It presents as red, pus-filled bumps and can affect individuals of all ages. If left untreated, it can lead to scarring. Treatment ranges from topical antibiotics for mild cases to oral antibiotics for more severe infections.
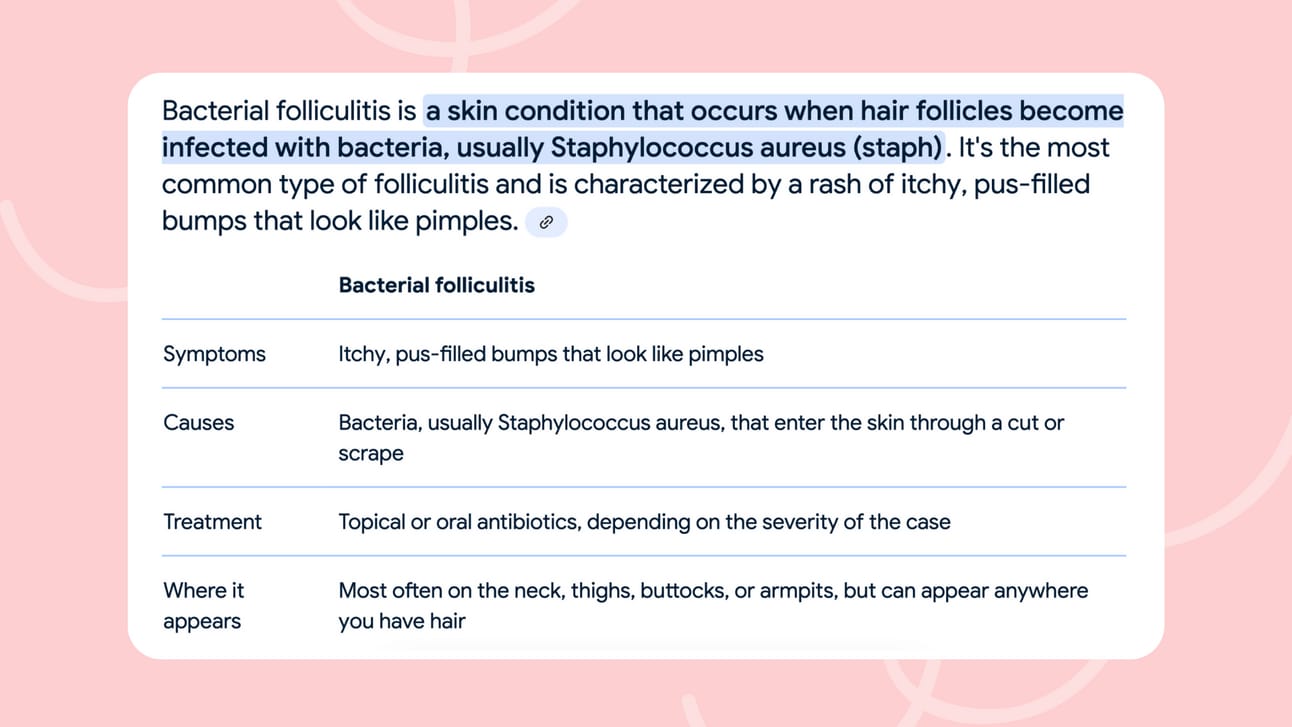
What is Bacterial Folliculitis?
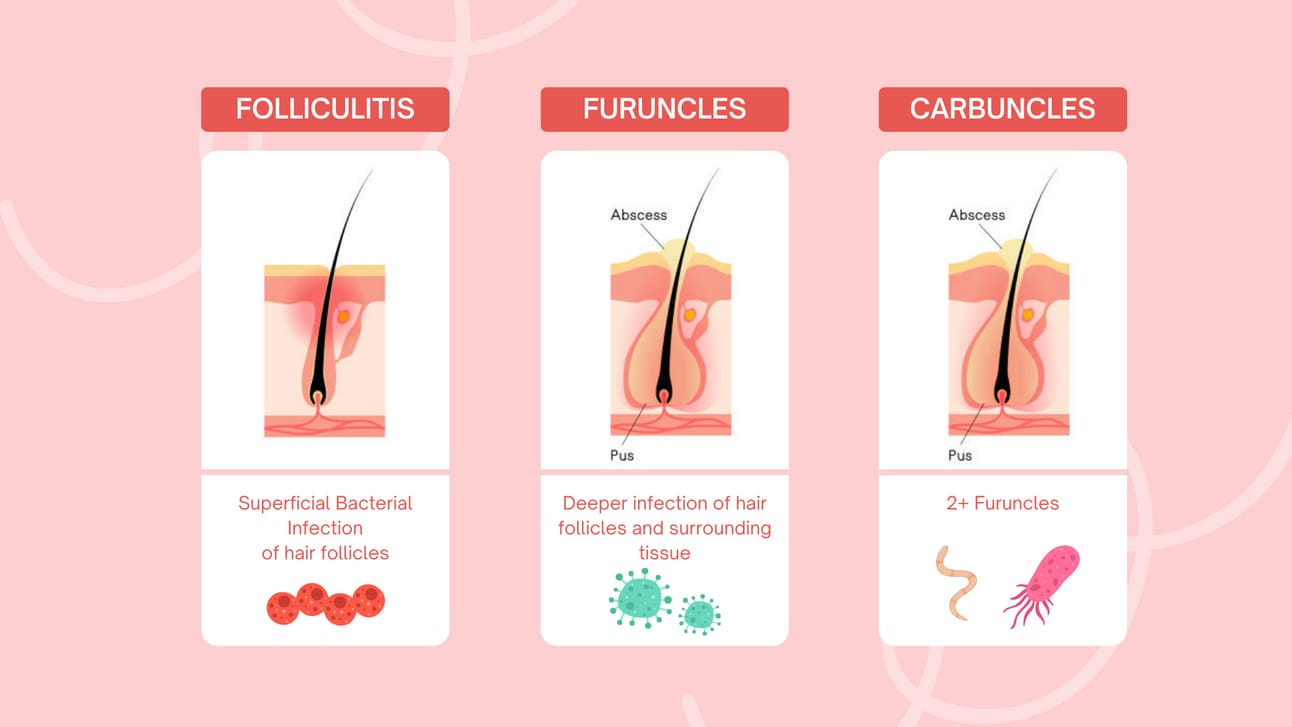
A bacterial infection affecting hair follicles, often presenting as:
Superficial: Involves the hair follicle's infundibulum, resulting in follicular papules and pustules.
Deep: Involves the subcutaneous fat, leading to furuncles (boils) and abscesses.
The initial event of folliculitis often follows mild trauma (e.g., aggressive shaving) or occlusion of the hair follicle.
Etiology: What Causes It?
The primary cause of bacterial folliculitis is infection with Staphylococcus aureus (gram-positive cocci). Other common bacteria can also be involved, but Staph aureus is the most frequent wrongdoer.
Autoinoculation: The infection can spread when a person scratches or shaves the infected area.
Recurrent Cases: If folliculitis keeps coming back, it's worth checking for nasal carriage of Staph aureus, which can be a source of infection.
Physical Exam: How to Identify It
When examining a patient, look for the following:
Common Areas Affected: Face, neck, groin, buttocks, chest, and armpits.
Characteristic Lesions: Look for follicular papules or pustules, sometimes with hair emanating from the pustule. Sometimes hair may be absent, though.
Tenderness: Superficial folliculitis tends to be non-tender, but deeper infections can be painful, involving tender pustules and nodules.

Treatment: Managing Bacterial Folliculitis
For Mild or Localized Infections:
Identifying any predisposing conditions that may cause follicular injury (shaving, scratching, etc.).
Use topical clindamycin or erythromycin twice a day (BID) for localized infections.
Betadine or chlorhexidine washes daily to the affected areas can help reduce bacterial load.
For Extensive or Resistant Infections:
If the infection is widespread or deep (like furuncles or abscesses), oral antibiotics are necessary to cover community-acquired MRSA (CA-MRSA).
Oral Antibiotics:
Doxycycline, minocycline, trimethoprim/sulfamethoxazole (Bactrim or Septra DS), and occasionally fluoroquinolones or beta-lactam-resistant penicillins (Dicloxacillin).
Treatment typically lasts 7-14 days.
Incision and Drainage: For furuncles (boils), it may be necessary to open the lesion and drain it. A culture and sensitivity test (C&S) should be done to guide antibiotic treatment.
Empiric therapy is also recommended. Start with MRSA antibiotic coverage, modifying based on culture results.
Special Considerations for Recurrent Folliculitis:
Nasal Carriage: If recurrent, nasal Staph aureus carriage should be considered. In such cases, use mupirocin intranasally twice daily for 5-10 days.
Non-Bacterial Folliculitis: If the infection is caused by Pityrosporum species (a type of fungus), fluconazole 200 mg daily for 10-14 days and ketoconazole shampoo 2% may be used for scalp involvement.
Post-Treatment Care and Follow-Up
Resolution: After treatment, pustules should resolve, and erythema (redness) will fade gradually. Post-inflammatory hyperpigmentation (PIH) may linger for some time but will eventually improve. Patients with darker skin types are likely to have PIH that persists.
Monitor for Recurrence: Keep an eye on patients for recurrence, especially in those with risk factors like nasal carriage or poor hygiene.
Prevention Tips
Avoid irritation by minimizing activities like aggressive shaving or scratching.
Maintain proper hygiene, including the use of antibacterial washes, to reduce the risk of folliculitis.
Summary
Bacterial Folliculitis is a treatable condition when caught early.
Topical treatments work well for mild cases; oral antibiotics may be needed for deeper infections.
Prevention involves reducing skin irritation and monitoring for recurrence.
Looking for more insights on managing and treating Common Bacterial Skin Infections like furunculosis, pseudofolliculitis barbae, cellulitis, erysipelas, and others?
↳ Check out our CE course on ‘Common Bacterial Skin Infections’ for in-depth strategies to enhance your clinical practice. 🧑🏻⚕️
📚 Why Choose Us for Your Continuing Education?
For all healthcare practitioners:
↳ Flexible learning: Fit your studies around your schedule.
↳ Real-world impact: Elevate your care with the latest in dermatology.
Earn your CE credits with one of the greatest educational platforms across the U.S!
💼 Career Development | Jobs
Looking to take the next step? Browse our Job Center for opportunities tailored to your goals.
Best aspect? You can find jobs both in primary and specialty care —we cater both. Filter by role, location, and more to best fit what you’re looking for.
🌎 Upcoming Dermatology Events
📅 December 2–3, 2024
📍 Boston, USA
Join experts from around the world to explore the latest breakthroughs in dermatology, skin disorders, and treatments. Connect with clinicians, researchers, and industry leaders as they discuss innovations in skin care, prevention, and emerging therapies.
🔎 Research Highlight
Skin Cancer Diagnosis by Lesion, Physician, and Examination Type: A Systematic Review and Meta-Analysis
Jennifer Y. Chen, MD, Kristen Fernandez, BS, Raj P. Fadadu, MD, MS, et al.
This systematic review highlights diagnostic accuracy for skin cancer based on lesion type, physician specialty, and examination methods. Dermatologists using dermoscopy achieved the highest accuracy, especially in melanoma diagnosis, with a 13.3-fold advantage over primary care physicians.
👋🏻 Until the next time
Thank you for being part of Beneath the Surface.
From expert advice to career inspiration, we’re here to support your journey in dermatology.
Keep exploring, keep learning, and let’s make strides in skin science together.
Stay curious, stay connected, stay DERM!
— The Derm for Primary Care Team
