Welcome back, DERM Community.
This week’s issue is brought to you by Decode.me
Last week, we explored scars and the biology behind their formation and treatment. This week, we're addressing something that might be quietly costing you patients without you even realizing it: telehealth, or the lack of it.
Here's the reality. Patients today expect convenience. They're accustomed to on-demand services in every other area of their lives. When your practice doesn't offer flexible virtual options, they find someone who does.
Telehealth is not just a pandemic-era workaround. It's a fundamental shift in how patients expect to access care. Despite its widespread adoption, misconceptions persist about when it works, why some implementations fail, and how to integrate it meaningfully into clinical practice without compromising quality.
Here's a detailed, evidence-informed look at telehealth from the infrastructure level to the clinic.
Understanding Telehealth: A Clinical Guide
Why Patients Are Walking Away
Before we dive into the mechanics, let's address the elephant in the room.
Patient expectations have permanently changed. Studies show that convenience, accessibility, and reduced travel time now rank among the top factors influencing where patients seek care. When a competitor offers video follow-ups and you require an in-person visit for a medication refill, patients notice. When a parent has to take a full day off work to bring a child in for a five-minute check, they remember.
This isn't about replacing excellent clinical care. It's about meeting patients where they are, literally.
How Telehealth Actually Works
Telehealth is the delivery of health care services remotely through telecommunications and information technology. It encompasses far more than video visits.
The telehealth ecosystem includes several distinct modalities:
Synchronous (real-time) – Live video or audio communication between patient and provider
Asynchronous (store-and-forward) – Transmission of clinical data, images, or information for later review
Remote patient monitoring – Continuous or periodic capture of physiologic data outside traditional settings
Mobile health (mHealth) – Smartphone apps, wearables, and sensors integrated into care delivery
Effective telehealth requires more than technology. It demands reliable broadband, appropriate platforms, clinical workflows designed for virtual encounters, and patients who can access and navigate the system.
What clinicians notice:
Early adoption challenges with technology and workflow integration
Gradual improvement in efficiency and patient satisfaction over 3–6 months
Or, in some cases, persistent barriers that undermine implementation
Infrastructure matters, but clinical design matters more.
Not All Telehealth Is the Same

Why Some Telehealth Programs Fail
When administrators ask, "Why isn't this working?", the answer is rarely just one factor.
Common contributors:
Inadequate broadband infrastructure or unreliable connectivity
Poor technology literacy among patients or providers
Lack of integration with existing electronic health records
Insufficient reimbursement or unclear regulatory frameworks
Privacy concerns and platform security vulnerabilities
Failure to account for patients with hearing, visual, or cognitive limitations
Here's a key insight: the first 3–6 months of implementation are critical. This is when workflows are established, staff are trained, and patient trust is built. Miss that window, and telehealth becomes a burden rather than an asset.
Evidence-Based Applications
Primary care and pediatrics
School-based telehealth programs increase access to primary care
Particularly effective for behavioral health and developmental assessments
Studies show high diagnostic agreement between remote and face-to-face methods
Specialty consultation
Cardiology: Remote ECG transmission, implantable device monitoring, heart failure management
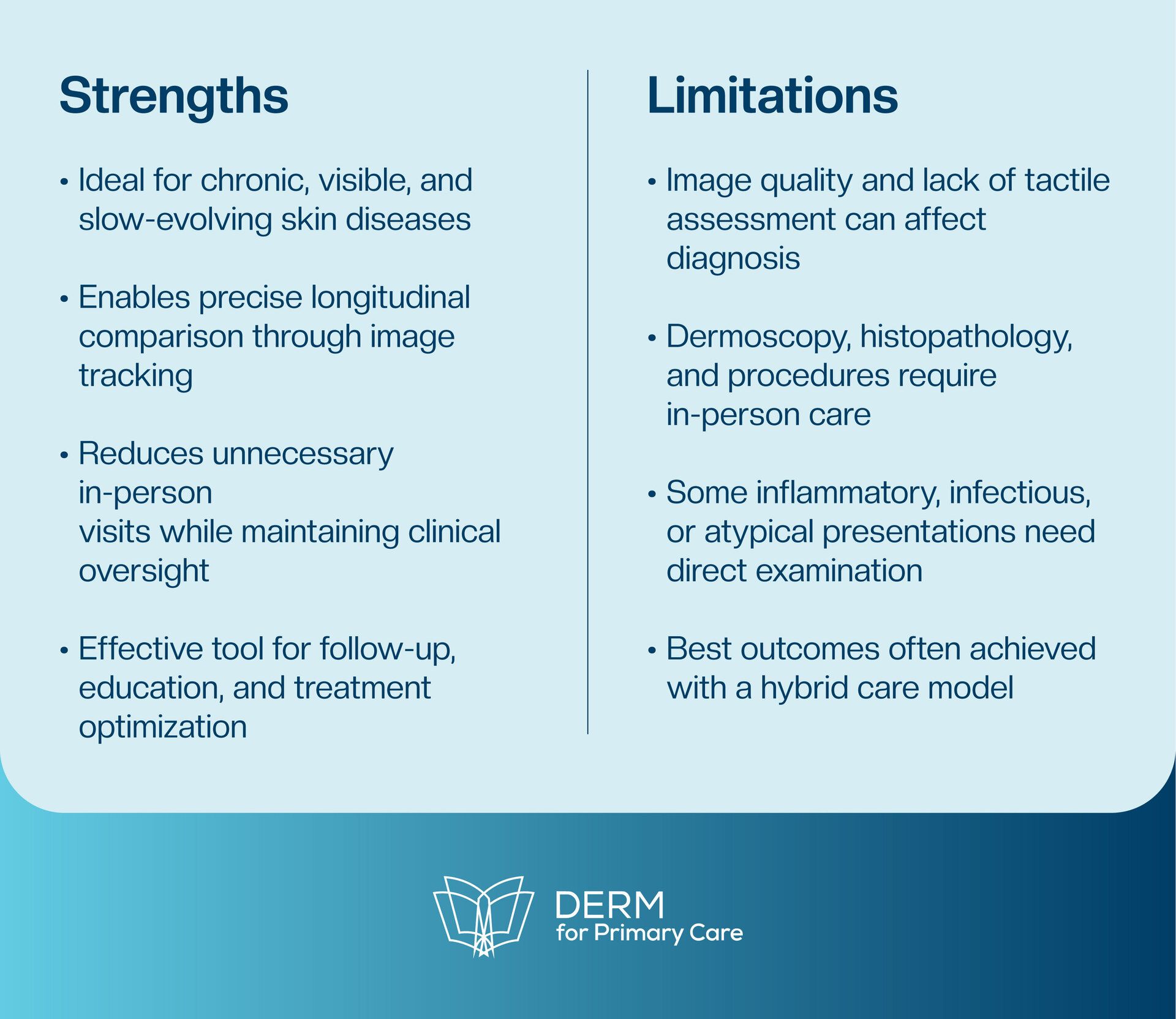
Dermatology: Store-and-forward image review for triage and diagnosis
Neurology: Stroke assessment and tele-rehabilitation
Chronic disease management
Heart failure: Implantable pulmonary artery sensors reduce hospitalizations
Diabetes: Remote glucose monitoring with real-time feedback
Hypertension: Home blood pressure monitoring with medication titration
Remote patient monitoring
Wearables and sensors for continuous physiologic data capture
Alerts and triggers for early intervention before decompensation
No single modality works in isolation. The best outcomes come from integrated, multimodal telehealth strategies.
Managing Challenges and Setbacks
Expected and manageable:
Initial technology learning curves
Occasional connectivity issues
Scheduling and workflow adjustments
Concerning but addressable:
Digital divide affecting vulnerable populations
Privacy breaches on unsecured platforms
Provider burnout from screen fatigue
Systemic barriers:
Licensure restrictions across state lines
Inconsistent reimbursement policies
Lack of standardized quality metrics
True telehealth failure is rare. More often, the issue is insufficient infrastructure investment, poor workflow design, or misalignment between modality and clinical need.
Practical Tips for Better Outcomes
Who Needs Extra Caution
Be thoughtful with patients who have:
Limited technology access or literacy
Hearing, visual, or cognitive impairments
Unstable medical conditions requiring hands-on assessment
Privacy concerns or insecure home environments
Language barriers without adequate interpreter services
Telehealth equity is as important as telehealth efficacy. Listen closely.
Remember:
Patients aren't leaving because your clinical skills are lacking. They're leaving because access is inconvenient.
Telehealth is not a replacement for traditional care. It is an expansion of how we deliver it. When we understand the technology, the workflows, and the patient populations best served, we stop losing patients to competitors and start building sustainable, hybrid models of care that serve everyone better.
The most successful clinicians don't just adopt telehealth. They design it thoughtfully, implement it strategically, and adapt it continuously to meet their patients where they are.
Looking for a Job?
We got you.
Here are some job postings you may find interesting:
Nurse Practitioner/Physician Assistant for Residential Facility | Full Time | On-site | Mount Sinai Wellness• Dahlonega, GA - Apply Here
Neonatal Nurse Practitioner, Pediatric Neonatology | Full Time | On-site | UTMB Health • Galveston, TX - Apply Here
Nurse Practitioner for OBOT Clinic | Part Time | On-site | AppleGate Recovery • Williamsport, PA - Apply Here
Nurse Practitioner for OTP Clinic ($68-$75/hour) | Part Time | On-site | BAART Programs • Bennington, VT - Apply Here
Nurse Practitioner/Physician Assistant | Full Time | On-site | Consensus Health • Bridgewater Township, NJ - Apply Here
Want to Go Deeper?
Take one of our modules
Here is our featured course for today!
Book Recommendation of the Week
“The Digital Doctor: Hope, Hype, and Harm at the Dawn of Medicine’s Computer Age” by Robert Wachter
Inspiration of the Week
“Your most unhappy customers are your greatest source of learning.”
👋🏻 See you next Thursday, DERM community!
Telehealth works best when it's grounded in infrastructure, clinical judgment, and honest communication about its limitations. Patient retention improves when access improves. It's that simple and that complex.
Next week, we'll explore pigmentation disorders: why melasma laughs at quick fixes and how evidence-based approaches actually move the needle.
See you next Thursday, DERM Community.
— The Derm for Primary Care Team