Welcome back, DERM Community!
Last week, we closed the loop on sun damage, highlighting how everyday habits, like consistent sunscreen use, shape long-term outcomes.
This week, we’re turning our attention to a common yet often underestimated clinical challenge: abscesses.
Though they may appear straightforward, abscesses carry layers of complexity:
Pathogenesis driven by infection and host response
Treatment that goes beyond drainage
Prevention strategies that can drastically reduce recurrence
Let’s break down the essentials every clinician should master.
Featured on This Week’s Chapter:
Abscesses: Clinical Essentials
What They Are → Pathophysiology and common causes.
Treatment in Practice → Drainage, antibiotics, and tailored care.
Prevention Strategies → Hygiene, wound care, and risk reduction.
Clinical Benefits → Why early and proper management improves patient outcomes.
Dermatology News You Can Use → Two new articles shaping dermatology practice.
Book Recommendation → A fresh read to strengthen your clinical mindset.
Inspiration of the Week → Prevention at the core of care.
Abscesses: What You Need to Know
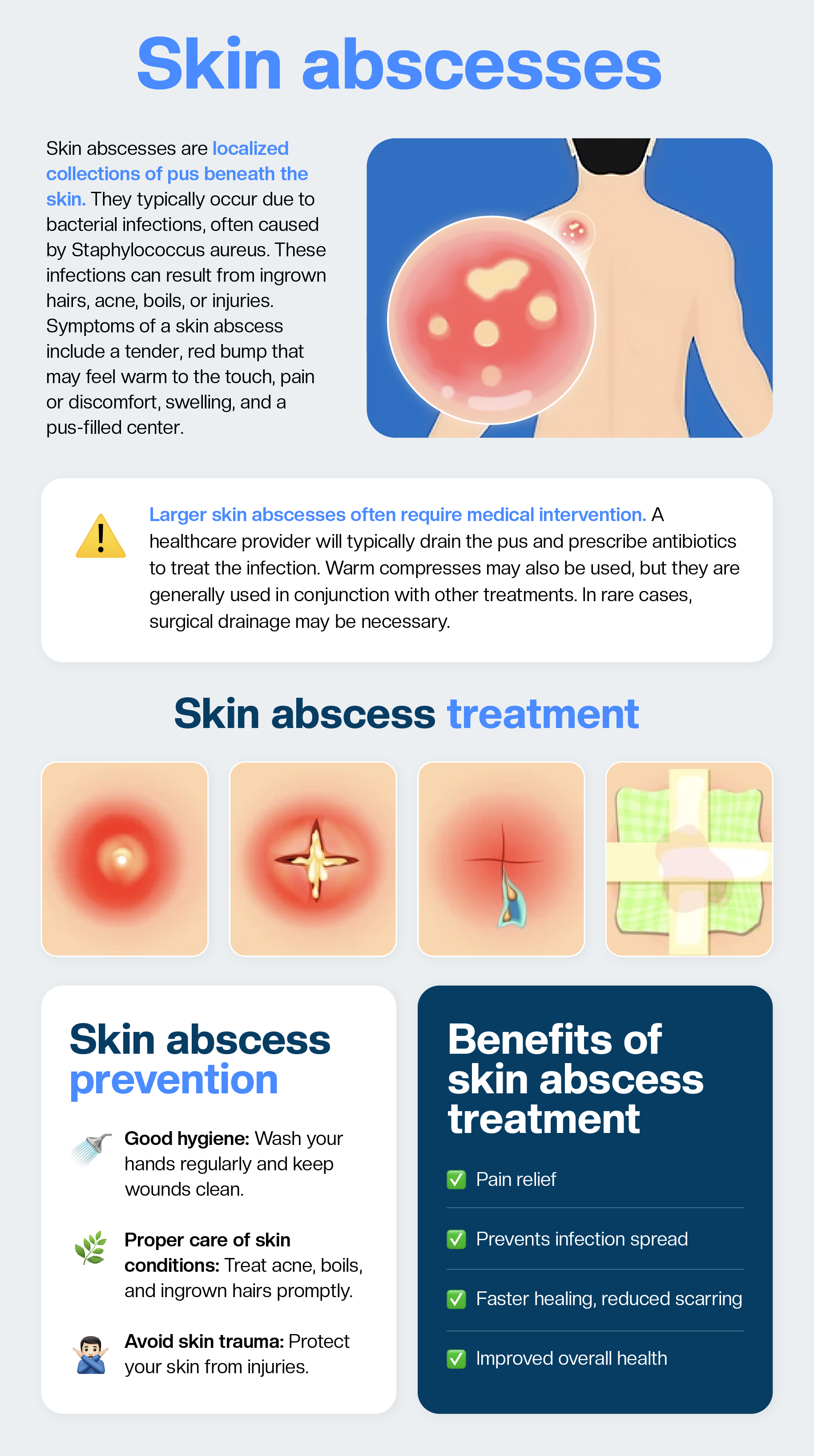
An abscess is a localized collection of pus caused by infection, often bacterial. They present with pain, swelling, warmth, and fluctuance. If untreated, abscesses can extend into deeper tissues or spread systemically.
Causes of Abscesses
Bacteria are the #1 culprit.
The most common cause is Staphylococcus aureus (including MRSA). Other frequent pathogens include Streptococcus spp., Escherichia coli, and Klebsiella pneumoniae, often depending on the abscess site.Anaerobes matter too.
Especially in perianal, oral, and deep tissue abscesses, where mixed aerobic–anaerobic infections are frequent.Underlying conditions increase risk.
Diabetes, immunosuppression, hidradenitis suppurativa, poor circulation, or skin barrier damage (cuts, trauma, insect bites) make abscess formation more likely.Location influences cause.
Skin & Soft Tissue: Staphylococcus aureus, Streptococcus spp.
Perianal/Abdominal: Gram-negative bacteria and anaerobes (e.g., Escherichia coli, Bacteroides spp)
Dental/Maxillofacial: Anaerobes, Streptococcus viridans group
Liver/Organ Abscesses: Escherichia coli, Klebsiella spp., occasionally parasites such as Entamoeba histolytica
Not always bacterial.
Fungi, parasites, or foreign-body reactions can also trigger abscess formation, though much less commonly.
Treatment Overview (see attached graphic):
Incision & Drainage (I&D): The cornerstone of management.
Antibiotics: Reserved for systemic signs, recurrent abscesses, or immunocompromised patients.
Adjunctive Care: Pain relief, wound care, and follow-up to monitor healing.
Early intervention prevents complications, reduces recurrence, and improves both patient comfort and clinical efficiency.
Clinical Pearls
Always rule out deeper or systemic infection before local treatment.
Not every abscess needs antibiotics, drainage is often sufficient.
Reinforce wound care instructions to patients for better healing.
Recurrence prevention = hygiene + managing risk factors.
We’ve Put Together a Free Guide Just for You!
Key Reads for Your Practice
Management of subcutaneous abscesses: prospective cross-sectional study (MAGIC)
How do hospitals really manage subcutaneous abscesses? This study reveals just how much practice varies, from the choice of anesthesia to whether cavities are packed or antibiotics prescribed.
The findings raise important questions about consistency, resources, and outcomes in abscess care.
A must-read if you want to see where everyday practice aligns (or clashes) with the evidence.
Read it here:
Optimization of Pathogen Detection in Abscess Specimens: A 6-Year Retrospective Study
Can we do better at identifying what’s really inside an abscess?
This study tested an optimized diagnostic protocol, combining culture, microscopy, acid-fast staining, and blood-culture enrichment, and found it boosted pathogen detection rates to 81.9%, a 20% improvement over conventional methods.
A compelling read for anyone managing infectious disease or microbiology workflows; showing how protocol refinements can directly improve diagnosis and patient care.
Read it here:
Book Recommendation of the Week
“Every Patient Tells a Story: Medical Mysteries and the Art of Diagnosis” by Lisa Sanders
Infections don’t always present as textbooks predict and that’s where clinical curiosity matters. In this book, Dr. Lisa Sanders takes readers inside real-life diagnostic puzzles, showing how abscesses, infections, and other common complaints can mask deeper issues.
Blending case stories with the science of medicine, she highlights the art of careful observation, patient history, and pattern recognition; skills every clinician can sharpen. A compelling read that reminds us why details matter in diagnosis and how listening to the patient often leads to the answer.
Inspiration of the Week
“The greatest medicine of all is to teach people how not to need it.”
-Hippocrates
👋🏻 See you next Thursday, DERM community!
This week, we explored abscesses: identification, treatment, and prevention.
Next week, we’ll take a closer look at scabies: how to recognize it, why it’s often missed, and the treatment strategies that actually work.
If today’s chapter gave you a sharper lens on abscesses, share it with your colleagues or trainees, they’ll thank you for it.
Thank you for being here with us!
— The Derm for Primary Care Team